Substance Use Disorder Treatment Plans
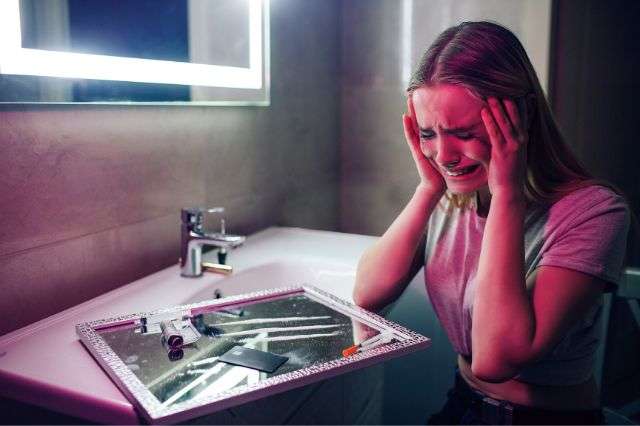
A healthy first step toward substance abuse recovery is creating a treatment plan with a provider. This personalized roadmap is going to help to set up realistic expectations, establish goals, and keep track of your progress. Treatment plans ought to consider how substance use affects … Read more